Let’s catch up!
They say spring is a time of growth and change, when unexpected surprises surface to face the sun! That is true for us at Perseverance, and as we adjust to our ever changing environment, we’d like to share some images from our social media pages to keep you visually entertained while sharing a bit of insight into our world!
Covid & Physiotherapy: Learning to Breathe Again
Navigating the Pandemic, Covid and Physiotherapy
“I worked with a 25 year-old Olympic athlete, fresh out of the hospital after being in an induced coma for three weeks. He had covid-19. After walking up 3 stairs, his heart rate was 210 beats per minute and he was completely winded.”
The journey to health for some people post covid is a long one. One of the topics that we are learning about at this stage of the pandemic is the lasting effects of COVID-19. Sometimes called “long-COVID, long-term COVID, or post-COVID”, this refers to the effects that can stay with a person after the virus is long gone. Persistent effects can be loss or limitation of the senses taste and smell, as well as cardiovascular symptoms, like drastically reduced cardio-capacity. Difficulty breathing, shortness of breath, or becoming winded after minimal physical activity are some of the symptoms that people are dealing with post covid. Re-training the body and the mind to get back the ability to breathe comfortably is where physiotherapy can play an important role.
Eric de Montarnal joined the Perseverance Physiotherapy & Wellness Team from one of the epicenters of COVID-19 back in 2020. Eric spent time working at the University of Alberta Hospital in Edmonton which is a city of a million people. The university is adjacent to a Medical Cardio-center, where patients who were critically ill with COVID were seeking rehabilitation after recovering from the worst of the virus.
Eric helped hundreds of patients learn to breathe again. “One of the initial aspects of this kind of physiotherapy is to start thinking of this as a cardiovascular challenge, instead of the virus, and therefore to manage our own fears around that.” says de Montarnal, “The mental aspect for these patients was just as important as the physical one. Imagine being completely winded after walking just a few steps: your heart is racing, you are breathing heavily, and you are scared. Working with these patients by monitoring their oxygen levels and coaching them through breathing is helpful, but also working with them to slowly build their endurance in a safe and supervised environment is really important.”
"Developing a plan to manage anxiety is a part of the work physiotherapists are doing in these cases, focusing on creating knowledge in these unchartered times is essential to successful rehabilitation. “We spend a lot of time educating patients on what to expect, what are red flags to watch for, and when to call for help.”
The physical part of therapy for covid-long patients includes working through exercises to engage the ribs and muscles, and practicing deep breathing techniques. de Montarnal encourages patients experiencing long-term effects of Covid not to lose hope. “At first this can seem really scary, but we need to treat this as an opportunity to re-learn the right ways to build cardio-fitness. Just like going for your first mountain bike ride, you can make progress with practice and support.”
The reality of our post-COVID world can feel daunting for many. If nothing else, it has forced us to put our health at the forefront of our minds, and for the fortunate ones, has reminded us that it is something to be grateful for. Physiotherapy is a practice that promotes and preserves health. Be it musculoskeletal, mental, or cardiovascular, a physiotherapist can help you work through your obstacles to get back to good health. So let’s take a breath, together.
Bones
Did you know that bones are teaming with life? They are not the washed-out, white material like the ones we stumble across on the side of a trail. That forest find is what remains once they are outside the body. Inside the body, they are a hive of activity, and are transforming, rearranging, and building new cells every second. They are also full of blood vessels and rich with life.
Bones have the ability to remodel themselves on a constant basis. Remodeling is the replacement of old bone tissue with new bone tissue. It involves the process of bone-building by cells called osteoblasts and bone resorption by cells called osteoclasts, which break down old bone. Once the bone has been broken down, the components of it (such as the mineral calcium), are distributed to the rest of the body through the bloodstream and used for other processes.
In the average healthy adult between 25-50 years of age, five to seven percent of bone mass is recycled every week. Turnover rates vary in different areas of the skeleton and in different areas of a bone. For example, the bone in the head of the femur may be fully replaced every six months, whereas the bone along the shaft is altered much more slowly.
Bone changes with Aging
Until about the age of 50, bone density tends to stay stable with equal amounts of bone formation and resorption. After age 50, bone resorption outpaces bone formation and bone loss often accelerates. This makes conditions such as osteopenia and osteoporosis more probable. Osteopenia is the precursor to osteoporosis which is a decrease in bone mass from low levels of calcium in the bone. This decrease in bone mass makes fractures more likely.
While this could seem discouraging, there are things that we can do to mitigate this process.
What can I do to keep my bones healthy?
Include physical activity in your daily routine:
Bone changes in response to the forces placed upon it, and therefore, your bone adapts by building more bone and becoming denser. Therefore, the more healthy stress you place upon your skeletal system the denser your bones will become.
Weight-bearing exercises, such as walking and jogging, and resistance exercises such as weight lifting can help you build strong bones and slow bone loss as you age.
Include plenty of calcium in your diet:
For adults aged 19 to 50 the Recommended Dietary Allowance (RDA) is 1,000 milligrams (mg) of calcium a day. The recommendation increases to 1,200 mg a day for women age 51 and older and for men age 71 and older. Good sources of calcium include dairy products, almonds, broccoli, kale, canned salmon with bones, sardines and soy products, such as tofu. Additional minerals important in bone health are phosphorous and magnesium.
Pay attention to your vitamin intake:
Your body needs vitamin D to absorb calcium. For adults ages 19 to 70, the recommended daily dose is 600 international units (IUs) a day. The recommendation increases to 800 IUs a day for adults age 71 and older. Good sources of vitamin D include oily fish, such as salmon, trout, whitefish, and tuna. Additionally, mushrooms, eggs, and fortified foods, such as milk and cereals. Sunlight also contributes to the body's production of vitamin D. Vitamin C and A are also important in normal bone growth. If you find it difficult to get enough vitamins and minerals from your diet, ask our Naturopathic Doctor about supplements.
Avoid or minimize substance use:
Don't smoke as it reduces the blood supply to your bones. If you are a woman, avoid drinking more than one alcoholic drink each day. If you are a man, avoid drinking more than two alcoholic drinks a day.
The best way to ensure bone health, is to pay attention to your diet, get moving, get lifting, and if you need help in determining the best way to do that, come and meet with one of our experienced therapists or our naturopathic doctor at Perseverance Physiotherapy and Wellness Center.
Written by Anja Roberts, PT
Websites referenced:
https://courses.lumenlearning.com/boundless-biology/chapter/bone/
https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/bone-health/art-20045060
Come back stronger: After Covid-19
Does COVID have you skipping the gym? Feeling unmotivated, having a hard time focusing, or lacking creativity? With the current events, how can we stay on track, or get back on track when there seems to be a certainty that we will be derailed again? Losing progress or gains can be discouraging!
At the moment everyone is experiencing different challenges while the world contends with the COVID-19 pandemic. We’ve all experienced ups and downs throughout this past year. Like many others, I struggled with the lack of motivation, depression, anger, frustration, unhealthy eating, restlessness and insomnia. As I’ve practiced my own coping strategies, I am thankful for my background in athletic therapy—it has given me an awareness of the human body, its systems, and how it performs and recovers. This in turn allows me to be intuitively aware of what my own body needs, be it to increase my water intake or electrolytes if I am feeling lethargic, or to know when I need a rest day, instead of pushing through my workouts. It has allowed me to rehab a running injury and start mountain biking and slack-lining to build my strength, balance, and allow me some time for meditation while I recover. Not to mention the pure enjoyment of playing outside.
These times require a pivot, coping skills and a fresh perspective. I am very excited to be able to help you attain some of these skills and awareness around your body and exercise. If we look at the big picture these negative feelings are unavoidable and at some point they are going to rear their head. The important part is to consider your coping mechanisms and whether they are healthy. Are you binge-eating because you are stressed? Can you not leave the house to go to the gym because of crippling anxiety? Or maybe over-exercising is your response to stress or anxiety. Coping mechanisms for stress are crucial, if the outside stressor is outside our control, we have to manage what we can influence—Exercise, eating well, adequate hydration, and healthier bedtime routines are all within our control, and can make a world of difference.
When a stressor this massive (global pandemic anyone?) is impacting our day to day lives the first things to go are proper fueling/healthy eating, sleep and exercise. The irony isn’t lost that these are the practices that help us combat this negative stress! If we can boost one of these the other two should naturally follow.
As an Athletic Therapist my goal is to help you boost the exercise and physical activity aspects of your life. We want to get back on track, because when we do we feel physically, emotionally and mentally better.
Athletic Therapy is not just treating the injury it is about treating the person as a whole. How can you be in your peak fitness if you cannot sleep? Without proper sleep your body cannot recover after hard workouts and the same if you are not fueling properly or if you are stressed about a friend or family member? All of it is connected so we as practitioners are treating much more than just an injury since these outside stressors will greatly impact the healing of your injury.
Athletic Therapy is a great idea for everyone, but during COVID it may be what you need to kick-start your active lifestyle or to maintain or motivate what you are already doing. Here are some of the things we can work on during a session whether you are a seasoned athlete or just starting a fitness routine for the first time:
1. Creating short term/ long term goals specific to you
2. While we create your program we will identify barriers that could keep you from these goals
3. Create healthy coping mechanisms and routines
4. Education on Performance and treatment while recovering from an injury
5. How to find a sport or activity that fits for you and creating a fitness program
Athletic Therapy is an as well as, an addition to, and not an instead of. The goal is to work together as a team on your goals, to get you where you want to be in your fitness sport or lifestyle. Not every program will have the same format, everyone has individual goals and interests. The true key is you enjoy what you are doing, so that it can be a part of your lifestyle and not just another passing fad.
-Cate
Taking a picture of back pain
INTRODUCTION: X-RAY’S, MRI’S & WEDDING PHOTOS
Imagine I show you a photo of a wedding I attended years ago with a group of 150 smiling faces. I ask you “please pick out who’s had the most to drink.” You don’t know anyone in the photo.
That would be a very tough task and one that you would likely get wrong. Why? Because it’s just a picture.
Surprisingly, this analogy is a good way to help us understand why we can’t confidently use your x-rays or MRI scans to explain back pain. A picture may be worth a thousand words – but when it comes to pain, it has its limits.
PART 1: PAIN-FREE PEOPLE HAVE “DISK DEGENERATION” TOO
When we feel a symptom, like pain, we want to make sense of that experience. We want to understand why we’re feeling that pain. “If only we knew what part of my back was causing my pain. The doctor could better treat the problem” we might think.
For decades healthcare providers have been ordering imaging for back pain sufferers in the hope of identifying the pain provoking structure. Roughly 25-50% of these scans are deemed inappropriate.
All the new technologies we have for peering into the human body are fantastic. They give us incredible detail of anatomy. Imaging techniques have even been saving lives since their invention. Scans are really good at finding fractures, infections & cancers for example – about 1% of all low back pain cases. With regard to back pain, why not take a look and see if anything is abnormal?
People are discovering why not. Scanning someone for pain is like a fishing trip, and since no one is perfectly “normal” you tend to find a lot of fish. If you look closely and often enough, almost everyone will have a little “degeneration” here or “disk bulge” there.
What would we find if we used an MRI machine and scanned a group of people without low back pain? This question was asked by a group of researchers in the U.S. and the study was published in the American Journal of Neuroradiology. Their results of more than 3000 pain-free people are provided in the image below.
The rows represent “abnormal” features found on the MRI scan and the columns represent the age of the participants. For example, if we look at the top left box, we see that 37% of pain-free 20-year-olds had “disk degeneration.”
If we look around the image some more, 50% of pain-free 40-year-old participants had “disk bulges.” 83% of pain-free 80-year-old participants had “facet degeneration.”
What sticks out is that the older we get, the higher chance we’ll have something found on a scan – even if we don’t have pain.
Researchers and clinicians are more commonly referring to these changes as “wrinkles on the inside.” These are normal signs of aging – not pain provoking structural changes to your tissues. If I start to get more noticeable wrinkles on my face, do I now have “face degeneration?” Will my face start to hurt?
It seems these imaging findings we’ve been using to explain someone’s pain doesn’t corelate to pain very well. It may help explain some specific conditions. However, for the vast majority of cases, we can’t confidently explain your low back pain based off of what we see on your scan alone. Why? Because many pain-free individuals have similar changes to their spines.
Many sober people can look like they’ve had a few cocktails before happy hour.
PART 2: SCANS CAN DO MORE HARM THAN GOOD
The language that’s used on X-Ray and MRI reports is catastrophic. Disk degeneration disease, disk space narrowing, facet arthrosis. Healthcare providers just throw these words at the patient like its meaningless. Meanwhile the patient is thinking “car tire, wear and tear! What do I do? I need to preserve it or replace it. So, I’m going to stop using it (ie avoid physical activity) or I’ll need spinal fusion!” They’ve got another 40 years on this planet, if their back is degenerating, they better preserve it, right?
The best recommendations for painful musculoskeletal conditions include exercise. Exercise is truly medicine. But exercise as a treatment makes little sense to a person that has been told by a doctor “it’s wear and tear.” If my back is “degenerating”, exercise would make it worse. Wouldn’t it? That is a sensible conclusion from the patient’s perspective.
Patients, now believing that their body is fragile and vulnerable, become less active. A vicious cycle of pain and disability begins. Less physical activity leads to more disability – more disability leads to more pain. This vicious cycle is a major reason one in five Canadian’s experience persistent pain.
In fact, a massive observational study including over 400,000 participants, published in the Journal of General Internal Medicine, had some eye-opening results.
Early MRI scanning was associated with higher rates of back surgery, greater use of prescription opioids, higher pain intensity and higher costs for treatment, compared to those without an early MRI scan. What good is that MRI doing?
PART 3: YOU’RE BROKEN, I’LL FIX YOU
Best practice guidelines for chiropractors recommend only taking x-rays when there are signs and symptoms of what we call “red flags.” Signs that indicate serious conditions. In the absence of red flags, X-rays are not recommended.
Yet there is a fraction of chiropractors that use routine X-rays to assess the structure and function of the spine. A practice dating back to 1910. Historically, these groups of chiropractors have argued that radiographs are helpful to measure postural abnormalities or identify vertebral misalignment and guide treatment with spinal manipulative therapy.
However, this practice has never been evaluated for its effectiveness. Considering all the potential harms I’ve discussed previously with imaging, understanding if routine X-ray use is something that chiropractors should continue to do is important.
Recently this has been of particular interest to the Chiropractic College of British Columbia (CCBC). The mission of the CCBC is to protect the public by regulating British Columbia’s doctors of chiropractic to ensure safe, qualified and ethical delivery of care. They reviewed the scientific literature to date to find out if routine X-rays were useful in managing patients with spinal pain.
The CCBC’s review concluded that there is “no evidence that the use of routine or repeat radiographs to assess the function or structure of the spine, in the absence of red flags, improves clinical outcomes and benefits patients…we recommend that chiropractors do not use radiographs for the routine and repeat evaluation of the structure and function of the spine.”
This comes to no surprise since we can’t confidently use pictures to explain someone’s pain.
CONCLUSIONS: PAIN IS COMPLEX & YOU ARE MORE THAN A PICTURE
It’s important to remember that many pain-free individuals have findings on their scan that sound scary, like degenerative disk disease. This isn’t a disease. I’m encouraged knowing that there are lot of smart researchers and public health advocates in the world trying to change the language healthcare providers use.
If you’ve had a scan that was used to explain your current back pain recently, who’s to say those “abnormal” findings weren’t there 2, 5, 10 years before you had pain.
Pain is extremely complex. A combination of infinite factors influence pain, like your fitness levels, sleep quality, mental stress, physical stress, mood, occupation, social economic status… the list goes on…. and on. But as a living, adaptable human-being, we can change the health of our tissues and effectively decrease pain in a variety of ways.
Dr. Iain Harrington is an evidence-based chiropractor with an interest in persistent pain.
To learn more about Dr. Iain, or to book an appointment, please visit the “Your Team“ page of our website.
Dr. Harrington is currently accepting new patients.
The truth about pelvic health
A Pelvis, you’ve got one, I’ve got one. So why is “Pelvic Health” Such a Secret?
About a quarter of all women are affected by pelvic floor disorders, according to a 2008 study published in the Journal of the American Medical Association.
The main risk factor is pregnancy.
Let’s just take a second to let that sink in. In a world where health risks are an intense part of our daily lives, add this to the list of things to worry about.
Put your hand up if pregnancy has ever been a part of your life. My hand is up, and for 75% of the women in my circle, their hands are in the air too. Out of that same group, how many can say that Pelvic Floor Rehabilitation has been a part of their lives post-baby. Number of hands in the air decrease to maybe one. WHY???
Part of the problem is (sssshhhhhh don’t say it too loud) that PEEING YOUR PANTS IS EMBARRASSING! We’ve been taught since our own days in diapers that peeing while not on the potty is bad. And you know what? It stuck. For those of us who have had the gift of pregnancy in our lives, many of us find that post-baby (whether via c-section or vaginial birth), a sneeze is dangerous, a coughing fit? Terrifying. A jog? Out of the question. Those triggers are some of the daily activities that induce involuntary ‘leakage’, the uncontrolled wee-wee in the undies. The results affect us mentally in a big way. Aside from just being inconvenienced by wet trousers, it can lead to all kinds of problems, from anxiety to weight gain.
Ok, now we’re going to let you in on something really good:
“Ninety per cent of cases of incontinence in aging women can be improved with exercise, and 70 per cent of cases can be treated with physiotherapy, according to a study by Chantal Dumoulin, a Canada research chair in urogynecological health and aging at the Université de Montréal.
Dumoulin says clinical practice guidelines indicate first-line treatment is supposed to be pelvic floor rehabilitation immediately after delivery.”
You are not alone, Mama, and yes, there is help for you.
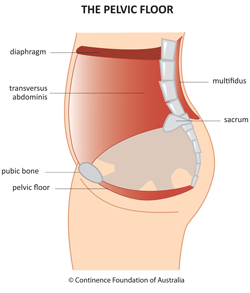
What is the pelvic floor?
The pelvic floor is the muscle group that fills the hole at the bottom of the pelvis. It contains the genitals, and acts as a hammock that holds up organs such as the bladder, uterus and rectum.
http://www.pelvicfloorfirst.org.au/pages/the-pelvic-floor.html
It's a part of the body many people don't think about, or maybe even know exists, until it starts not doing its job.
When the muscles become too weak or stretched, patients can suffer from urinary or fecal incontinence or a condition known as organ prolapse, when the organs held up by the pelvic floor drop, sometimes to the point of bulging out of the vagina.
So, yes. It is a thing. A thing that needs a little more attention. There have been women who have gone to the extreme of having surgery where an artificial ‘hammock’ is inserted into their bodies in order to alleviate the side effects we’ve talked about. The surgery is now banned in many countries, and in Canada surgical mesh implants used to treat pelvic organ problems were removed from the Canadian market following a safety review by Health Canada.
“The consequences of healthcare providers spending relatively little time with postpartum women have been well-documented in terms of missed mental health diagnoses, but the longterm effects on women’s bodies are also profound ― and often overlooked. The stress of a vaginal delivery can increase a woman’s risk of developing pelvic organ prolapse ― a painful condition in which her pelvic organs essentially fall out of place ― decades down the road.
But one country that is giving women’s postpartum pelvic health the attention it deserves? France. For decades, the French government has subsidized “perineal re-education,” i.e., physiotherapy that helps strengthen a new mother’s pelvic floor.”
New mothers in France can expect to receive a prescription for 10-20 sessions of “la rééducation périnéale”. Yet another example of something wonderful that we can learn from the french!
In Canada, many health insurance companies offer physiotherapy as a service covered under their plans, and this enables many women who have an extended health plan to seek pelvic health rehabilitation from a Physiotherapist. FOR FREE.
Pelvic Health is not only a subject that needs to be talked about more openly, it is a specialty that needs to be celebrated as an alternative to surgical intervention. Many women experience a drastic improvement or a complete resolution to their pelvic health issues with just a handful of sessions.
At Perseverance Physiotherapy & Wellness, we got pretty excited when we knew Rosemarie Sanche was coming into the picture. Not only is Rosemarie an excellent Physiotherapist, she is passionate, experienced, and extremely knowledgeable on the subject of pelvic health. Book a session with Rosemarie to explore how she can help you achieve better health today.
Rosemarie Sanche, PT
Written by Andy Lumanta
Sources: https://www.cbc.ca/radio/whitecoat/it-s-time-to-break-the-taboo-around-pelvic-floor-health-in-canada-say-advocates-1.5308972
https://www.huffingtonpost.ca/entry/what-the-french-get-so-right-about-taking-care-of-new-moms_n_587d27b4e4b086022ca939c4